
Gum disease, also called periodontitis, is a serious condition that can damage the gums and bone around your teeth. If left untreated, it can lead to tooth loss and affect your overall health. This guide will explain what causes gum disease, how it’s diagnosed, the signs to watch for, and how to prevent and treat it.
What Causes Periodontitis?
Periodontitis usually starts as gingivitis, a mild inflammation of the gums caused by a buildup of dental plaque—a sticky film of bacteria that forms on your teeth. If this plaque isn’t removed by brushing and flossing, it hardens into tartar, which can irritate the gums.
In addition to plaque, there are several systemic and local factors that can increase the risk of gngivitis:
- Smoking: Smoking can mask the signs of gingivitis by reducing blood flow to the gums, making it harder to detect inflammation.
- Hormonal Changes: Hormonal fluctuations during puberty, menstruation, pregnancy, or from using oral contraceptives can increase gum sensitivity and lead to exaggerated responses to plaque.
- Poor Nutrition: Vitamin C deficiency (scurvy) and other nutritional factors can weaken the immune system and make gums more susceptible to infection.
- Diabetes: Poorly controlled diabetes, especially type 1 diabetes in children, can make gums more prone to inflammation.
- Medications: Certain drugs, such as those used for seizures or hypertension, can cause gum overgrowth, making it harder to maintain oral hygiene.
As the infection worsens, it turns into periodontitis, which not only affects the gums but also the deeper tissues and bones that support the teeth. The body’s immune response to the bacteria causes inflammation, leading to damage of the bone and tissues that hold the teeth in place.
Signs and Symptoms of Periodontitis
Early gum disease (gingivitis) can be mild, so it’s easy to overlook. However, as the disease progresses to periodontitis, more serious symptoms will appear. Sings and symptoms include:
- Red, swollen, or tender gums
- Bleeding gums when brushing or flossing
- Bad breath or a bad taste in your mouth that doesn’t go away
- Receding gums (gums pulling away from the teeth, making teeth look longer)
- Loose or shifting teeth
- Pain when chewing
- Deep pockets between the teeth and gums
- Changes in how your teeth fit together when biting
Diagnosing Periodontitis
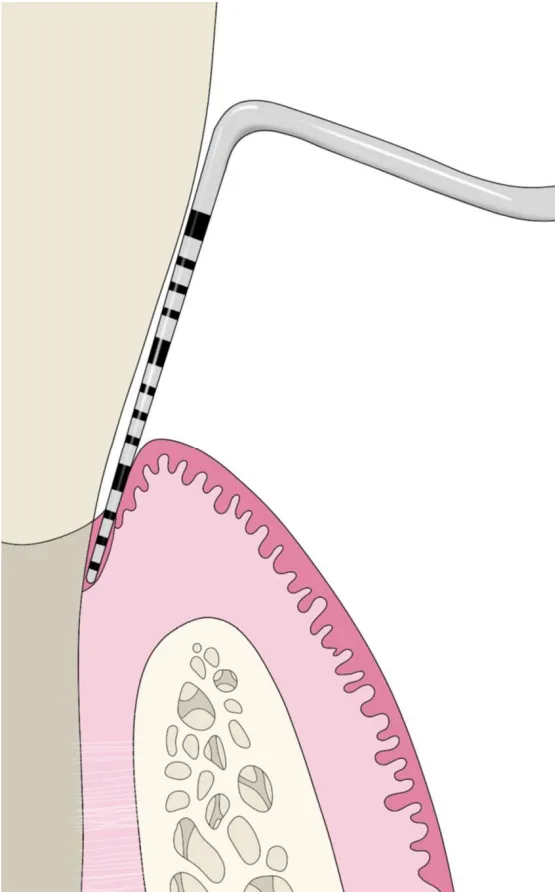
Dentists diagnose periodontitis using a mix of periodontal probing, visual examination, radiographic examination, and understanding your overall health history. Generally, this starts by measuring how deep the spaces (pockets) are between your teeth and gums using a small tool called a periodontal probe (pictured below). They also check for signs of gum recession, where the gums pull back and expose the roots of your teeth. These two measurements together create a measurement known as clinical attachment loss.
In 2017, a new classification system for periodontitis was introduced, incorporating staging and grading to better reflect the severity and complexity of the disease, as well as the risk of its progression.
Stages
Staging is based on the severity of the disease and the complexity of managing it. It is primarily determined by the extent of clinical attachment loss, radiographic bone loss, and tooth loss due to periodontitis.
- Stage 1 (Mild): Slight swelling of the gums with small pockets between the teeth and gums. No significant bone damage yet.
- Stage 2 (Moderate): Gums are more swollen and bleeding is common. Some bone loss is visible on X-rays, and deeper pockets are present.
- Stage 3 (Severe): There is significant gum recession, deeper pockets, and more bone loss. Teeth may start to feel loose.
- Stage 4 (Advanced): Severe bone loss, loose teeth, and major gum recession. The teeth may be at risk of falling out, and surgery may be needed to save them.
Grading
Grading assesses how quickly the disease progresses, risk factors, and the response to treatment. It is divided into three categories:
- Grade A: Slow progression with minimal bone loss or attachment loss.
- Grade B: Moderate progression, which is the default grade unless evidence suggests faster or slower disease progression.
- Grade C: Rapid progression with significant bone loss or attachment loss over a short period. Risk factors such as smoking or uncontrolled diabetes often shift the grading toward Grade C.
Preventing and Managing Gum Disease
Once a patient has periodontitis it can not be completely cured, only managed. The damage done by periodontitis can then be altered using treatments such as bone grafting, implants, dental crowns, dental bridges, and extractions. This is why taking care of your gums is crucial for preventing gum disease and managing it if you already have it. Here are some key steps to follow:
- Brush Your Teeth Twice Daily: Use fluoride toothpaste and a soft-bristled toothbrush to clean your teeth thoroughly.
- Floss Daily: This helps remove plaque and food particles from between your teeth where your toothbrush can’t reach.
- Regular Dental Cleanings: Professional cleanings by a dentist or hygienist are essential in removing tartar and addressing gingivitis before it progresses.
- Rinse with Antibacterial Mouthwash: This can help reduce bacteria in your mouth.
- Healthy Diet: Consuming a balanced diet rich in vitamins and minerals, especially vitamin C, can help strengthen your immune system and maintain gum health.
Conclusion
Periodontitis is a serious condition that affects not just your mouth but your overall health as well. By recognizing the signs early, maintaining good oral hygiene, and getting regular dental checkups, you can prevent or manage gum disease effectively.
If you think you might have gum disease, don’t wait to see your dentist. Early treatment can save your teeth and protect your health.
Disclaimer
The contents of this website, such as text, graphics, images, and other material are for informational purposes only and are not intended to be substituted for professional medical advice, diagnosis, or treatment. Nothing on this website constitutes the practice of medicine, law or any other regulated profession.
No two mouths are the same, and each oral situation is unique. As such, it isn’t possible to give comprehensive advice or diagnose oral conditions based on articles alone. The best way to ensure you’re getting the best dental care possible is to visit a dentist in person for an examination and consultation.
SAVE TIME AND MONEY AT ANY DENTIST

Less dental work is healthier for you. Learn what you can do to minimize the cost of dental procedures and avoid the dentist altogether!

