Gingivitis is a mild but common form of gum disease that causes irritation, redness, and swelling (inflammation) of your gingiva, the part of your gum around the base of your teeth. While gingivitis itself is not severe, it can lead to more serious gum diseases like periodontitis if left untreated. Recognizing the signs and understanding how to prevent and manage gingivitis can go a long way in maintaining oral health.
What Causes Gingivitis?
The main cause of gingivitis is dental plaque, a sticky, colorless film that forms on your teeth when bacteria in the mouth mix with food particles and saliva. When plaque is not removed properly through regular brushing and flossing, it hardens into tartar, or calculus, which further irritates the gums and leads to inflammation. If left untreated, plaque-induced gingivitis can progress to periodontitis, a more severe form of gum disease that can result in tooth loss.
In addition to plaque, there are several systemic and local factors that can increase the risk of gingivitis:
- Smoking: Smoking can mask the signs of gingivitis by reducing blood flow to the gums, making it harder to detect inflammation.
- Hormonal Changes: Hormonal fluctuations during puberty, menstruation, pregnancy, or from using oral contraceptives can increase gum sensitivity and lead to exaggerated responses to plaque.
- Poor Nutrition: Vitamin C deficiency (scurvy) and other nutritional factors can weaken the immune system and make gums more susceptible to infection.
- Diabetes: Poorly controlled diabetes, especially type 1 diabetes in children, can make gums more prone to inflammation.
- Medications: Certain drugs, such as those used for seizures or hypertension, can cause gum overgrowth, making it harder to maintain oral hygiene.
Signs and Symptoms of Gingivitis
Gingivitis can be easy to miss in its early stages, especially in smokers, where inflammation can be masked by reduced blood flow. Some key signs to watch for include:
- Swollen or puffy gums
- Dark red or purplish gums
- Gums that bleed easily when brushing or flossing
- Bad breath (halitosis)
- Receding gums or gums that pull away from the teeth
Types of Gingivitis
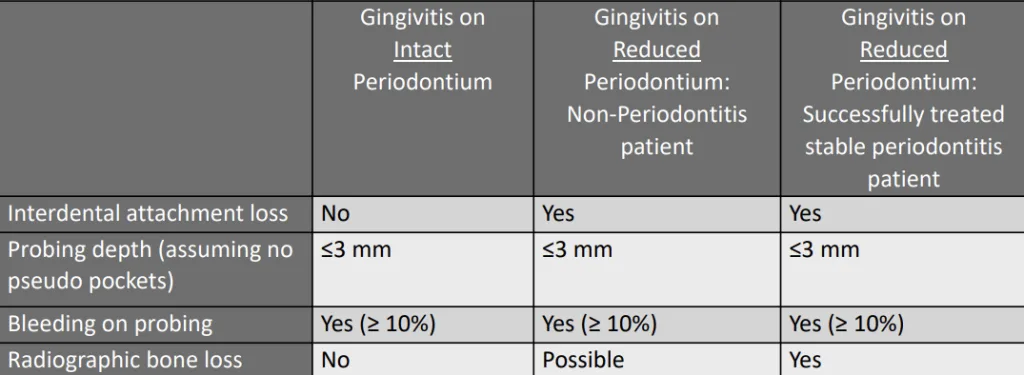
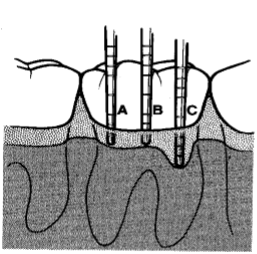
Gingivitis manifests differently based on the health of the supporting tissues around your teeth. Dentists will mainly use periodontal probing (pictured below) to determine what type of gingivitis you have, and what treatment you should receive. There are three main categories of gingivitis based on the periodontium (the tissues supporting the teeth):
- Gingivitis on an Intact Periodontium:
- This type occurs in people with no previous history of periodontal disease. The gums may become red, swollen, and prone to bleeding.
- Signs: Bleeding on probing (BOP), but no attachment loss (between tooth and gums) or bone loss is detected.
- Gingivitis on a Reduced Periodontium (Non-Periodontitis Patients):
- This occurs in patients who do not have periodontitis but have experienced bone loss due to other factors, such as orthodontic treatment or tooth extraction.
- Signs: Attachment loss with a probing depth of less than 3 mm, but no signs of active periodontitis.
- Gingivitis on a Reduced Periodontium (Successfully Treated Periodontitis Patients):
- This occurs in patients who have had successful treatment for periodontitis, but the gums have not fully recovered. While the gingiva may appear healthy, these patients are at higher risk of recurrence.
- Signs: Interdental attachment loss, probing depths of 3-4 mm, and the possibility of radiographic bone loss. Bleeding on probing can be present if inflammation recurs.
The Progression from Gingivitis to Periodontitis
Gingivitis does not always progress to periodontitis, but it can if it is left untreated. The progression is generally broken down into four stages based on Page and Schroeder’s pathogenesis of periodontal disease:
- Initial Lesion:
- Appears within 2-4 days of plaque accumulation.
- There is an increase in gingival crevicular fluid (GCF) flow, and polymorphonuclear neutrophils (PMNs) are the primary immune cells involved.
- This stage is not clinically apparent but can be seen histologically as the beginning of an immune response.
- Early Lesion:
- Occurs between 4-7 days, correlating with early gingivitis.
- There is an increase in capillary proliferation, leading to erythema and bleeding on probing.
- Lymphocytes become more prominent, and up to 70% of collagen surrounding the infiltrated area is destroyed.
- Established Lesion:
- Appears after 2-3 weeks, representing chronic gingivitis.
- The blood vessels become engorged, and blood flow slows down, leading to a bluish hue on the reddened gingiva.
- Plasma cells dominate the immune response, and there is a significant loss of collagen.
- Advanced Lesion (Periodontitis):
- This stage represents the transition from gingivitis to periodontitis.
- The inflammation extends to the alveolar bone and periodontal ligament, resulting in bone loss and the formation of periodontal pockets.
Preventing and Managing Gingivitis
Gingivitis is preventable and manageable with good oral hygiene practices:
- Brush Your Teeth Twice Daily: Use fluoride toothpaste and a soft-bristled toothbrush to clean your teeth thoroughly.
- Floss Daily: This helps remove plaque and food particles from between your teeth where your toothbrush can’t reach.
- Regular Dental Cleanings: Professional cleanings by a dentist or hygienist are essential in removing tartar and addressing gingivitis before it progresses.
- Rinse with Antibacterial Mouthwash: This can help reduce bacteria in your mouth.
- Healthy Diet: Consuming a balanced diet rich in vitamins and minerals, especially vitamin C, can help strengthen your immune system and maintain gum health.
Conclusion
Gingivitis is a reversible condition with proper care and attention. If you experience symptoms like gum bleeding or swelling, it’s essential to seek professional advice early to prevent progression to more severe gum diseases like periodontitis. Adopting a diligent oral hygiene routine and understanding risk factors can significantly improve your gum health and overall well-being.
Disclaimer
The contents of this website, such as text, graphics, images, and other material are for informational purposes only and are not intended to be substituted for professional medical advice, diagnosis, or treatment. Nothing on this website constitutes the practice of medicine, law or any other regulated profession.
No two mouths are the same, and each oral situation is unique. As such, it isn’t possible to give comprehensive advice or diagnose oral conditions based on articles alone. The best way to ensure you’re getting the best dental care possible is to visit a dentist in person for an examination and consultation.
SAVE TIME AND MONEY AT ANY DENTIST

Less dental work is healthier for you. Learn what you can do to minimize the cost of dental procedures and avoid the dentist altogether!

